Upcoming Enhancements to the Electronic Prior Authorization for Drugs
Effective Jan 1, 2021, CareFirst BlueCross BlueShield and CareFirst BlueChoice, Inc. (CareFirst) is upgrading its Prior Authorization (PA) notification system through the Provider Portal. The newly enhanced system offers easy to read dashboards, a user-friendly interface and electronic communication with CareFirst clinical staff.
This upgrade is being released throughout 2021 starting first with Medicare Advantage (MA) members in January and will be available for all members in mid-2021.
What Does This Mean for You?
CareFirst Direct will look different. After logging into the Provider Portal and selecting the Prior Auth/Notification tab, you will see a new PA Notification Home Screen. This new screen will be available as soon as Dec. 19.
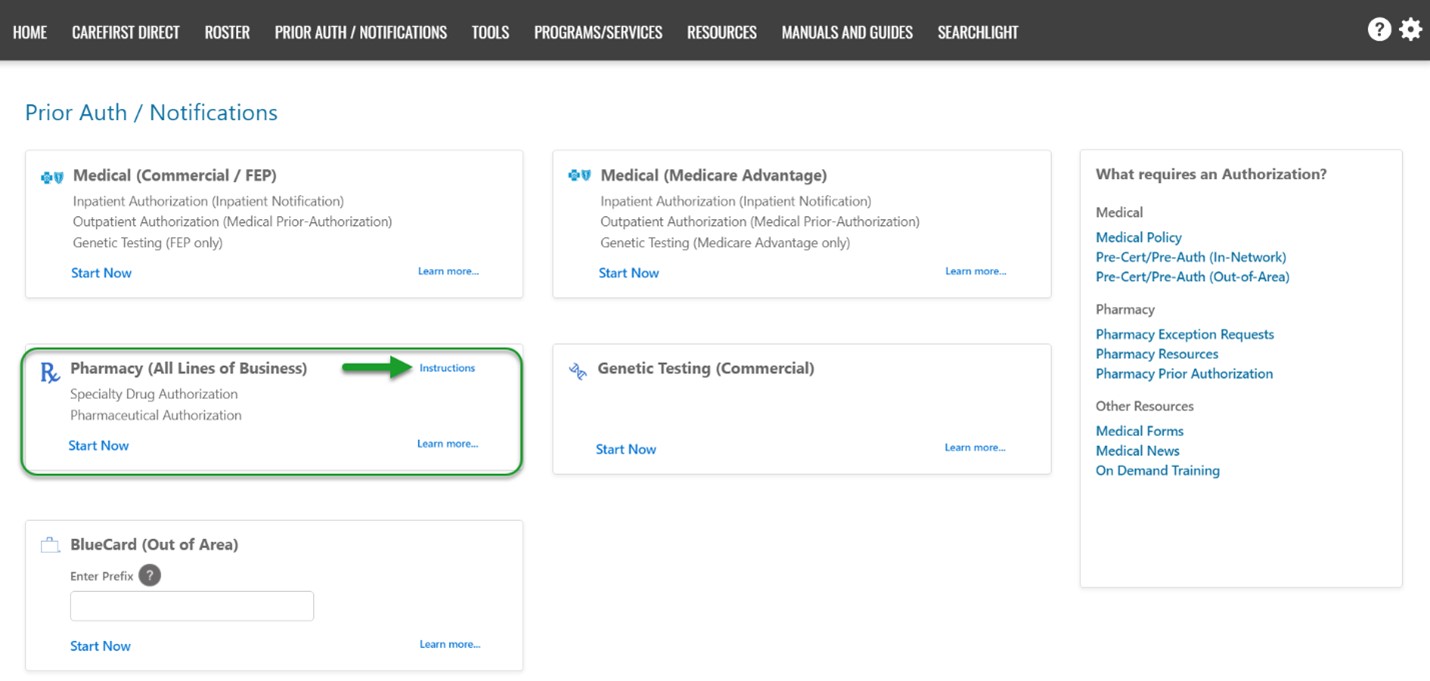
For Drug PAs, you will click on “Start Now” within the “Pharmacy (All lines of business)” section. Then you will be taken to the new PA notification system to complete your request. When you enter your request, you will notice that several screens have been eliminated in CareFirst Direct. This makes the process easier and more convenient. Click on ‘Instructions’ to learn how to enter PAs using this more efficient process.
After beginning your request in CareFirst Direct, you will be directed to Novologix.
Currently, you can still use the Medical (Commercial/FEP) section to enter PAs. However, this capability will be retired by mid-2021. Using the new process will provide you with the best experience when submitting drug PAs and prepare you for the changes coming in 2021.
Note: The changes in CareFirst Direct will not impact the way you enter authorization information in Novologix.
If you have questions about this change, contact your Provider Relations Representative.
