Important Update on the New Authorization/Notification System
Utilization Management Flexibility
On January 6, CareFirst BlueCross BlueShield and CareFirst BlueChoice, Inc. (collectively “CareFirst”) shared how we’re reducing administrative burden by temporarily relaxing utilization management policies for hospitals ceasing non-urgent procedures.
We are pleased to see COVID hospitalization trends decreasing in recent days. CareFirst will maintain these flexibilities through the end of the month to allow these facilities to prioritize recovery from the surge. Standard utilization management policies will resume for all facilities after February 28.
System Open Through February 28
We are also continuing to make adjustments to our systems to assist you in providing care to your patients when they need it most. Starting February 14, 2022 through February 28, 2022, the authorization/notification system will open, allowing you to enter authorizations for dates of service January 7, 2022 and after. We recognize there have been some challenges in entering authorizations within the standard 3-day and 7-day windows for outpatient and inpatient authorizations/notifications. To assist you with this, we will be lifting those guidelines during this time so that you can enter your authorizations that have fallen outside of the normal guidelines.
Important Note: The guidelines lifted during this time applies to Commercial, FEP and Medicare Advantage members whose authorizations/notifications are entered into Altruista Guiding Care. Medicaid authorization systems are not impacted.
- Log in to provider.carefirst.com
- Select the Prior Authorizations/Notifications tab
- Click ‘Start Now’ in the Medical (Commercial/FEP/Medicare Advantage) section
- Select the type of request you need (Inpatient or Outpatient), ensuring you enter authorizations with a date of service no earlier than 1/7/2022.
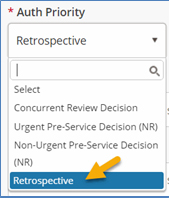
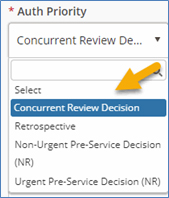
- Select the appropriate ‘Auth Priority’ and complete the remaining fields to submit your authorization. (See Additional steps below for details).
Additional steps
For outpatient authorizations:
- ‘Retrospective’ should be selected if the authorization is submitted after the ‘Auth Start Date’.
For inpatient authorizations:
- ‘Retrospective’ should be selected if the authorization is submitted after the member has been discharged.
- ‘Concurrent Standard’ should be selected if the authorization is submitted after the ‘Admit Date’, but before the member has been discharged.
For additional information on entering authorizations that fall outside of the 3-day and 7-day windows for outpatient and inpatient authorizations/notifications review our Frequently Asked Questions document.
No Auth Required Notification Update
In addition, in the coming weeks, you will notice that the authorization/notification system will alert you more often when an authorization you are entering is not required. The system will not allow you to move forward in the process.
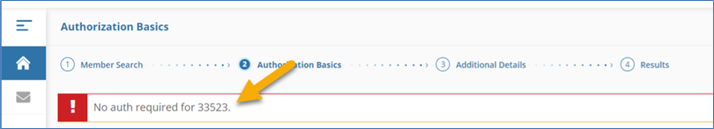
How to determine if an authorization is required?
It is important to utilize CareFirst Direct as well as other supporting online resources available to assist you in identifying when authorizations are required for your patients. Please review this user guide for assistance.
Educational Resources Available
We continually update our Frequently Asked Questions document, so check back regularly. Be sure to check out all training available on the new authorization/notification system under the Courses by Topic section on the Center for Provider Education site.
Thank you for your continued partnership and patience as you become acquainted with the new authorization/notification system. We will keep you updated on any new developments and resources.
