New District of Columbia Infertility Legislation Effective January 1, 2025
Effective January 1, 2025, District of Columbia law (B25-34) requires that fully insured DC individual and group health plans (including grandfathered plans) provide coverage for the diagnosis and treatment of infertility, including, artificial insemination, in vitro fertilization, and standard fertility preservation services. Self-insured plans may opt in to these benefits. Treatment must be consistent with the physician’s or surgeon’s overall plan of care.
Definitions included in this legislation:
ASRM means the American Society for Reproductive Medicine.
Infertility means a disease, condition, or status characterized by:
- The failure to establish a pregnancy or to carry a pregnancy to live birth after regular, unprotected sexual intercourse in accordance with the guidelines of ASRM.
- A person’s inability to reproduce without medical intervention either as a single individual or with their partner; or
- A licensed physician’s findings based on a patient’s medical, sexual, and reproductive history, age, physical findings, or diagnostic testing.
Standard fertility preservation services means procedures that are consistent with established medical practices or professional guidelines published by ASRM or the American Society of Clinical Oncology for a person who has a medical condition or is expected to undergo medication therapy, surgery, radiation, chemotherapy, or other medical treatment that is recognized by medical professionals to cause a risk of impairment to fertility.
Treatment for infertility means procedures consistent with established medical practices in the treatment of infertility by licensed physicians and surgeons, including diagnosis, diagnostic tests, medication, surgery, or gamete intrafallopian transfer.
Requirements of the legislation:
- Cost sharing (copayment, coinsurance and deductible) for infertility services will be applied to the same extent as cost sharing provided for other like services. For example, an infertility lab service would have the same cost share as other non-infertility lab services.
- Coverage for in vitro fertilization is limited to three (3) complete egg retrievals with unlimited embryo transfers from the eggs retrieved or from any egg retrieval performed prior to January 1, 2025, per member’s lifetime with CareFirst.
- Fertility enhancing drugs will be covered under the prescription drug benefits.
- Benefits will not be limited based on arbitrary factors, such as number of attempts, dollar amounts or age.
- Benefits will be provided for medical costs related to an embryo transfer made from a member to a third party (surrogate or gestational carrier). Benefits will not be provided for any medical costs of a third party beyond the embryo transfer procedure.
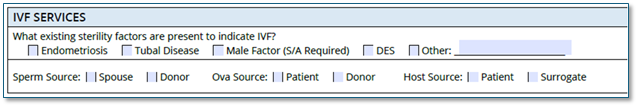
To adjudicate claims and apply benefits appropriately, providers must complete the Assisted Reproductive Technology Pre-Treatment Request form. For embryo transfers, please be sure to indicate on the form that the Host Source is a surrogate if a surrogate is used.
As always, be sure to check benefits and eligibility on CareFirst Direct or CareFirst On Call.
