Available Now: New Prior Authorization Lookup Tool
We are excited to announce that the new Prior Authorization Lookup Tool is now available for you to access to assist in determining which services you provide require authorization. The implementation of this tool is something our provider community has asked for to help streamline the authorization process, and it is officially here and available for you today!
How will I access the new tool?
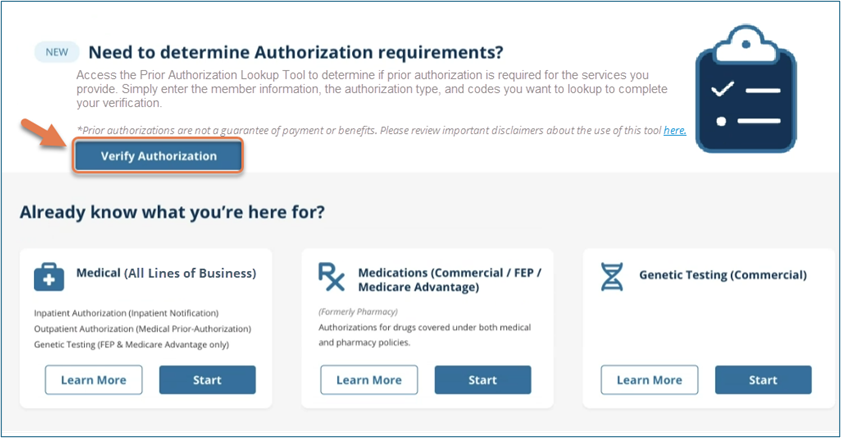
This tool is located on the ‘Prior Authorization/Notification’ landing page once logged into the CareFirst Provider Portal and serves as a quick way to verify authorization requirements before entering a request.
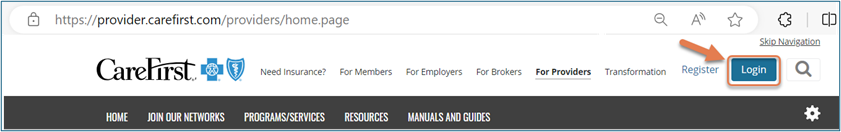
- Navigate to provider.carefirst.com and login.
- Select the Prior Auth / Notifications tab.

- Click Verify Authorization.
What are the key features?
- User friendly interface where you can quickly enter required information to determine if a prior authorization is required.
- A clear ‘Yes’ or ‘No’ response for prior authorization requirements.
- Ability to enter multiple service codes for the same member.
- When applicable, a direct link to the appropriate prior authorization system to enter your request.
- The ability to print the response for your records.
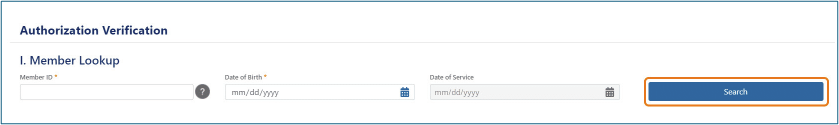
What information do I need to complete a verification?
Simply enter the member information (member ID and date of birth) to pull up their policy information.
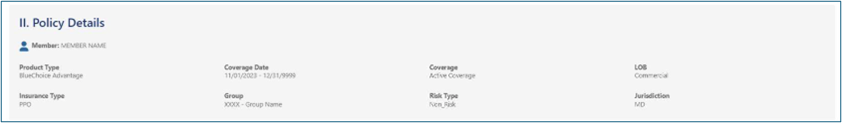
You can then enter the authorization type, place of service, and codes you want to look up to complete your verification. (You are able to search for multiple codes by selecting 'Add More')
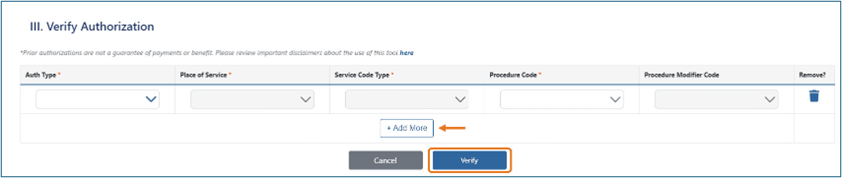
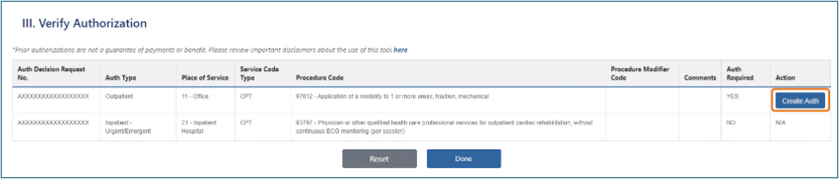
Once you select 'Verify', you will be provided with an Auth Decision Request No. for your records, and a summary of your search results that includes a Yes or No response in the 'Auth Required' field and, in most case, a direct link to the appropriate authorization portal to enter your request.
Is training available?
Yes! You can access our Walk-through for more information about how to access and utilize the new Prior Authorization Lookup Tool.
