MedStar Select Plan Update
Effective January 1, 2022, the MedStar Select plan will be administered by CareFirst BlueCross BlueShield (CareFirst).
Who is impacted?
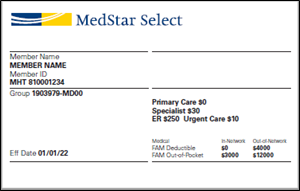
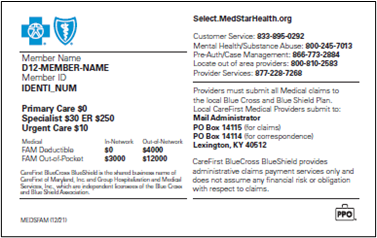
CareFirst commercial members participating in the MedStar Select plan, identified by the plan name on their CareFirst member ID card.
- All MedStar Select members will be receiving new identification cards.
- Please check the back of the card for updated health plan contact information for service, claims, medical, behavioral health and substance use disorder.
|
|
|
What do you need to know?
Claims Submission
- For services rendered up through December 31, 2021, claims should continue to be sent to:
- Electronic Submission: Payer ID 251MS
- Mail paper claims to: MedStar Claims, PO Box 1200, Pittsburgh, PA 15230-1200
- Claims for dates of service rendered on and after January 1, 2022, must be submitted to CareFirst as you usually do. For more information on submitting claims, refer to Chapter 5: Claims, Billing and Payment from the Provider Manual and our on-demand training module, Submitting Claims for Medical Providers.
Authorizations
- Any prior authorizations for services in 2022 that are submitted prior to December 31, 2021, should be sent to Evolent to manage.
- Authorizations entered for members beginning on January 1, 2022, must be submitted through CareFirst’s authorization portal on carefirst.com, except when the authorization spans multiple plan years, as described below:
- For all inpatient stays authorized prior to January 1, 2022, and the stay spans the transition period, you can continue to submit claims to UPMC for MedStar Select at discharge. Claims submitted after June 30, 2022, must be submitted to CareFirst.
- For all inpatient stays authorized before January 1, 2022, and the stay spans the transitions, call Evolent’s utilization management (UM) team through discharge. The Evolent UM team can be reached by phone at 855-242-4875 and fax at 855-431-8762.
- Important Note: If Evolent approved an authorization in 2021 for a procedure in 2022, CareFirst will honor that authorization. Members do NOT need a new authorization.
Appeals
- Any appeals for services rendered through December 31, 2021, should continue to be sent to the following address:
- MedStar Provider Appeals, PO Box 269, Pittsburgh, PA 15230-0269
- Any appeals submitted after January 1, 2022, should be submitted to the following addresses:
|
Professional Providers |
Institutional Providers |
Behavioral Health
- CareFirst will also begin supporting behavioral health and substance use services for these members effective January 1, 2022.
- Contact CareFirst’s Mental Health and Substance Abuse line at 800-245-7013. Select option 2 for assistance with mental health support services and care management.
- For dates of service starting January 1, 2022, authorizations for these services must be submitted through the provider portal on provider.carefirst.com.
Additional Information
Eligibility and benefits information for MedStar Select members can be accessed through CareFirst Direct starting January 1, 2022.
Questions?
Please reach out to your Provider Relations Representative.